What is Lipedema?
Surgery may be necessary to remove or restore the damaged skin, particularly if it is very thick, dark, or scarred, or if it affects a bodily part such as the genitalia or the anus and impairs its ability to function. A knife, a laser, or a skin transplant may be used during surgery to remove or replace the injured skin. Surgery can enhance the skin's look and functionality, but it can also have unfavorable side effects including bleeding, infection, or scarring. As such, it ought to be reserved for extreme circumstances and should only be suggested by a dermatologist.
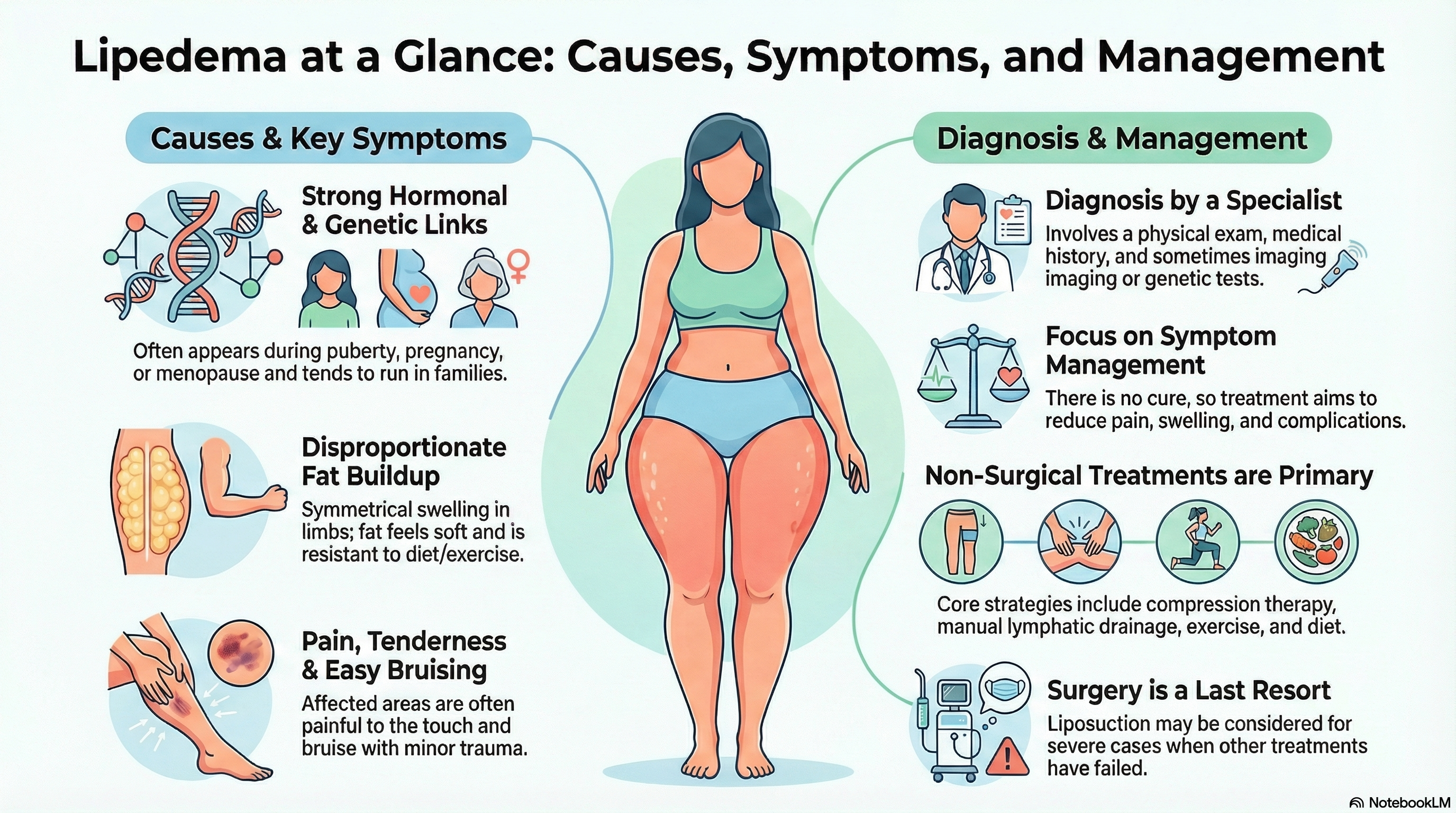
Causes of Lipedema
The exact cause of lipedema is not known, but it may involve several factors, such as:
-
Hormonal factors: During times of hormonal transition, such as adolescence, pregnancy, or menopause, lipedema frequently appears or gets worse. Because it may alter the body's fat distribution and metabolism, the female sex hormone estrogen may be involved in the onset and course of lipedema.
-
Genetic factors: Since lipedema has been known to run in families, certain individuals may be predisposed to developing the illness. Mutations in some genes, such as the HSD17B12 gene, which is involved in the manufacture of estrogen, have been linked in some studies to lipedema.
-
Environmental variables: Lifestyle factors that can impact the health and function of the lymphatic system, which is in charge of removing waste products and excess fluid from the tissues, include food, exercise, stress, and trauma. These factors can also have an impact on lipedema.
Symptoms of Lipedema
The primary sign of lipedema is the accumulation of fat in the arms, legs, and occasionally the torso that does not go away with diet or exercise. The fat may feel chilly or delicate to the touch, and it may look mushy, doughy, or dimpled. The limbs that are impacted by the fat may also appear swollen, heavy, or out of proportion to the rest of the body. Additional signs of lipedema might be:
-
Pain, swelling, or stiffness in the affected limbs, especially after standing, walking, or sitting for long periods of time.
-
Bruising, bleeding, or infection of the affected skin, especially after minor trauma or injury.
-
Reduced mobility, balance, or range of motion of the affected limbs can affect daily activities and quality of life.
-
Psychological distress, such as anxiety, depression, or low self-esteem, is due to the physical and emotional impact of the condition.
Diagnosis of Lipedema
Lipedema can be diagnosed by a doctor who specializes in vascular or lymphatic disorders, such as a phlebologist or a lymphologist. The diagnosis may involve:
-
Medical history and physical examination: The physician will inquire about the patient's current medicines or therapies, as well as the development and course of any symptoms, personal and family history of lipedema or other associated disorders. Along with examining the afflicted limbs, the doctor will search for lipedema-related symptoms such skin changes, bruises, swelling, or extra fat.
-
Imaging tests: To evaluate the structure and function of the lymphatic system and blood vessels in the affected limbs, as well as to rule out other conditions like lymphedema, obesity, or venous insufficiency that may cause similar symptoms, the doctor may use imaging tests like lymphoscintigraphy, MRIs, or ultrasounds.
-
Genetic testing: To look for mutations in particular genes, including the HSD17B12 gene, which may be linked to lipedema, the doctor may perform genetic testing. Genetic testing can identify individuals who are at risk of acquiring lipedema, such as family relatives of afflicted persons, and can also assist in confirming the diagnosis of lipedema.
Treatment of Lipedema
There is no cure for lipedema, but treatment can help manage the symptoms and prevent complications. The treatment of lipedema may include:
-
Compression treatment: It is done by applying pressure to the injured limbs using clothing such as bandages, sleeves, or stockings in order to lessen bruising, discomfort, and swelling. Additionally, compression treatment helps stop lipedema from getting worse by enhancing lymph and blood circulation.
-
Manual lymphatic drainage: It is a kind of massage that aids in the removal of extra fluid and waste from the tissues by stimulating the lymphatic system. Additionally, manual lymphatic drainage can enhance skin health and mobility while lowering discomfort, bruising, and edema.
-
Exercise: This includes engaging in physical activities that help maintain a healthy weight, develop muscles, and improve lymph and blood flow. Examples of these activities include walking, swimming, and cycling. Exercise can also enhance happiness and quality of life while lowering pain, stiffness, and edema.
-
Diet: This entails maintaining a healthy, balanced diet that is high in nutrients and low in calories. It may also help reduce weight gain and offer antioxidants and anti-inflammatory compounds that can shield cells from inflammation and damage. In addition to improving skin health and immunity, diet helps lessen bruising, discomfort, and edema.
-
Medicine: To aid with lipedema symptoms, including discomfort, swelling, or bruising, the doctor may give medicine such as diuretics, anti-inflammatories, or painkillers. Medication side effects, however, might also include bleeding, dehydration, and upset stomach. As a result, it is important to utilize medicine carefully and under a doctor's supervision.
-
Surgery: To reduce the extra fat in the afflicted limbs and enhance their look and functionality, the doctor could advise a lipectomy or liposuction. Moreover, surgery can stop the development of lipedema and lessen bruising, discomfort, and swelling. On the other hand, problems from surgery might also result in scars, bleeding, or infections. Consequently, surgery ought to be reserved for extreme cases in which all other avenues of treatment have failed.
Prevention of Lipedema
There is no way to prevent lipedema, as it is a genetic disorder that is present from birth. However, some measures can be taken to reduce the risk or severity of lipedema, such as:
-
Avoiding or treating any hormonal imbalances, such as low estrogen or high testosterone levels, that may trigger or worsen lipedema, by consulting with a doctor and taking hormone replacement therapy or other medications as prescribed.
-
Avoiding or minimizing any environmental factors, such as stress, trauma, or infection, that may affect the health and function of the lymphatic system and cause inflammation or damage to the tissues, by practicing relaxation techniques, getting enough sleep, or seeking medical attention as needed.
-
Getting regular check-ups and screenings for any signs of lipedema, such as swelling, bruising, or skin changes, by visiting a doctor who specializes in vascular or lymphatic disorders, and undergoing imaging tests or genetic tests as recommended.





