What is Acid Reflux?
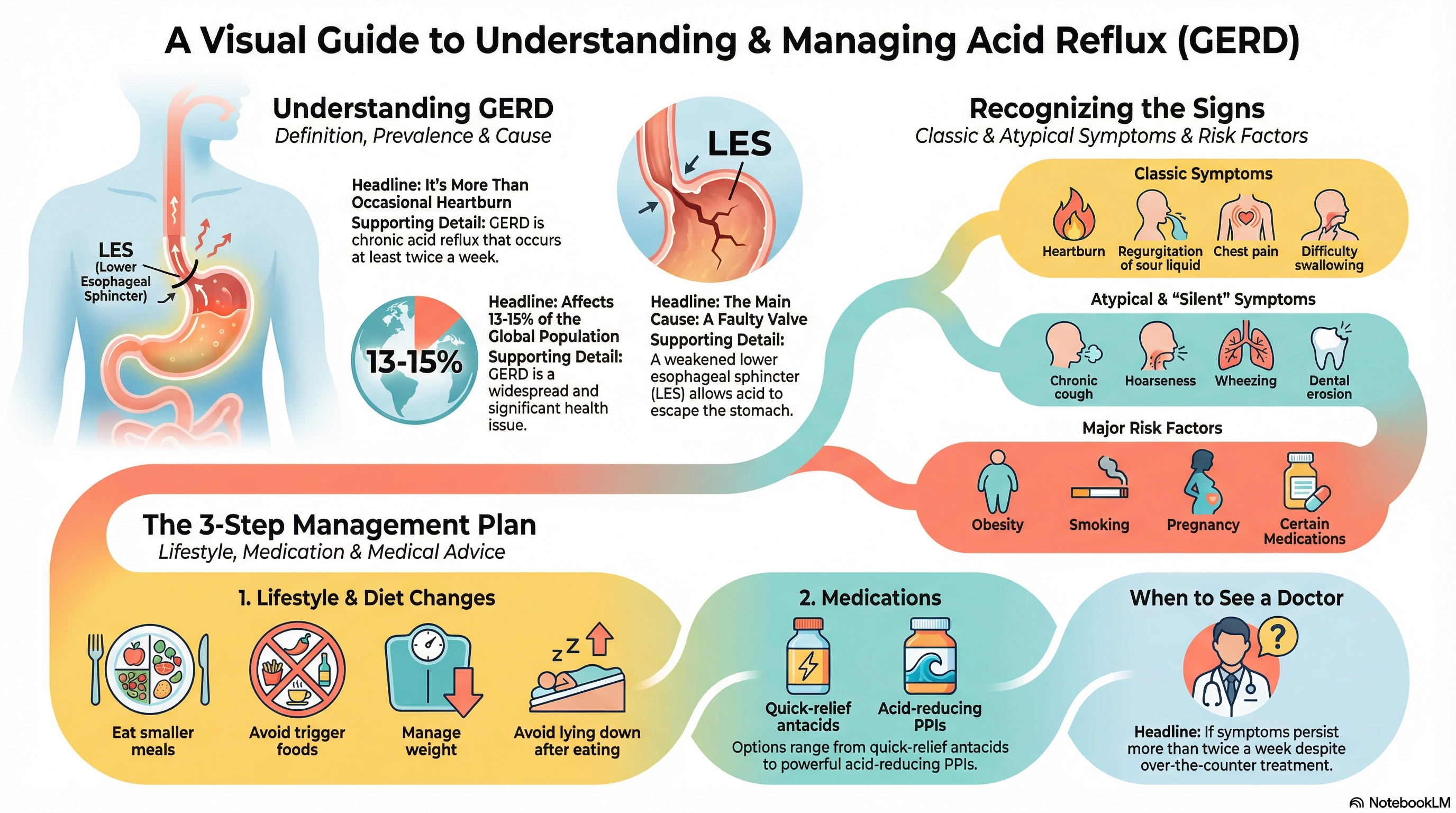
Acid reflux occurs when stomach acid or bile flows backward (regurgitates) into the esophagus—the tube that connects your throat to your stomach. While many people experience occasional reflux, it is classified as Gastroesophageal Reflux Disease (GERD) when it occurs frequently (twice or more per week) or causes significant symptoms and potential complications.
GERD is a common condition, with a prevalence of approximately 13–15% worldwide. It significantly impacts health-related quality of life and, if left untreated, can lead to serious conditions such as Barrett’s esophagus, a precancerous change in the esophageal lining.
Causes of Acid Reflux
The primary cause of acid reflux is a dysfunction of the lower esophageal sphincter (LES), the muscular ring that acts as a valve between the esophagus and the stomach.
-
LES Malfunction: The LES may become weakened or relax inappropriately (transient relaxations), allowing acid to escape upward.
-
Hiatal Hernia: A common anatomical factor where a portion of the stomach pushes through the diaphragm into the chest, disrupting the LES function.
-
Increased Abdominal Pressure: Factors such as obesity, pregnancy, or wearing tight clothing can physically push stomach contents back into the esophagus.
-
Delayed Gastric Emptying: When food stays in the stomach too long (common with fatty meals), it increases the pressure and likelihood of reflux.
-
Lifestyle & Genetic Factors: Tobacco smoking, certain medications (like NSAIDs), and genetic predispositions can all contribute to the weakening of the esophageal barrier.
Symptoms of Acid Reflux
Symptoms of acid reflux can vary widely between individuals and are categorized into typical and "extra-esophageal" symptoms.
-
Heartburn and Regurgitation: The cardinal signs are a burning sensation rising toward the neck and the effortless return of sour or bitter liquid into the mouth.
-
Chest Pain: This can often mimic the pain of a heart attack. Always rule out cardiac causes first if you experience unexplained chest pressure.
-
Difficulty Swallowing (Dysphagia): A sensation of food being stuck or trouble moving food down the esophagus.
-
Atypical Symptoms: Chronic cough, hoarseness (especially in the morning), sore throat, wheezing, and dental erosion from acid contact.
-
Silent Reflux: In some cases, damage occurs to the throat or airways without the patient feeling traditional heartburn.
Diagnosis of Acid Reflux
Diagnosis typically begins with a review of your symptoms and how you respond to initial treatments, but several tests may be used to confirm GERD:
-
Upper Endoscopy (EGD): A procedure where a small camera is used to visualize the esophagus for signs of inflammation (esophagitis), ulcers, or Barrett's esophagus.
-
24-Hour pH Monitoring: This is considered the "gold standard" for diagnosis, measuring the actual amount of acid exposure in the esophagus over a 24-hour period.
-
Esophageal Manometry: This test assesses the pressure and muscle function of the LES and the esophagus.
-
Barium Swallow: An X-ray imaging test used to identify structural issues like strictures or hiatal hernias.
Treatment of Acid Reflux
Treatment focuses on managing symptoms, healing the esophageal lining, and preventing long-term complications.
-
Lifestyle & Dietary Changes: This is the first line of defense. It includes eating smaller meals, avoiding "trigger" foods (spicy, fatty, caffeine, alcohol), and waiting 2–3 hours after eating before lying down.
-
Medications: * Antacids: For quick, temporary relief.
-
H2 Blockers: To reduce acid production for 6–12 hours.
-
Proton Pump Inhibitors (PPIs): The most effective for long-term acid suppression and healing.
-
-
Surgical Options: For severe cases unresponsive to medication, procedures like Nissen Fundoplication (wrapping the stomach around the LES) or the LINX device (a magnetic bead ring) can surgically reinforce the reflux barrier.
Prevention of Acid Reflux
While some factors like genetics cannot be changed, many lifestyle adjustments can significantly reduce the risk and severity of reflux:
-
Maintain a Healthy Weight: Reducing abdominal fat decreases the physical pressure on your stomach.
-
Sleep Elevation: Use a wedge pillow or bed risers to elevate the head of your bed by 6–8 inches, using gravity to keep acid down at night.
-
Quit Smoking: Smoking weakens the LES and reduces the production of saliva, which helps neutralize acid.
-
Mindful Eating: Avoid overeating and identify your personal triggers by keeping a food and symptom diary.
-
Avoid Late-Night Snacking: Ensure your last meal is at least three hours before bedtime to allow for proper gastric emptying.





