What is Barrett's Esophagus?
Under normal conditions, the esophagus is lined with flat, pale cells called squamous epithelium. When these cells are chronically exposed to stomach acid and bile, the body may attempt to protect itself by replacing those cells with tougher, "columnar" cells that contain goblet cells. These salmon-pink cells are better equipped to handle acid but carry a risk of becoming cancerous over time.
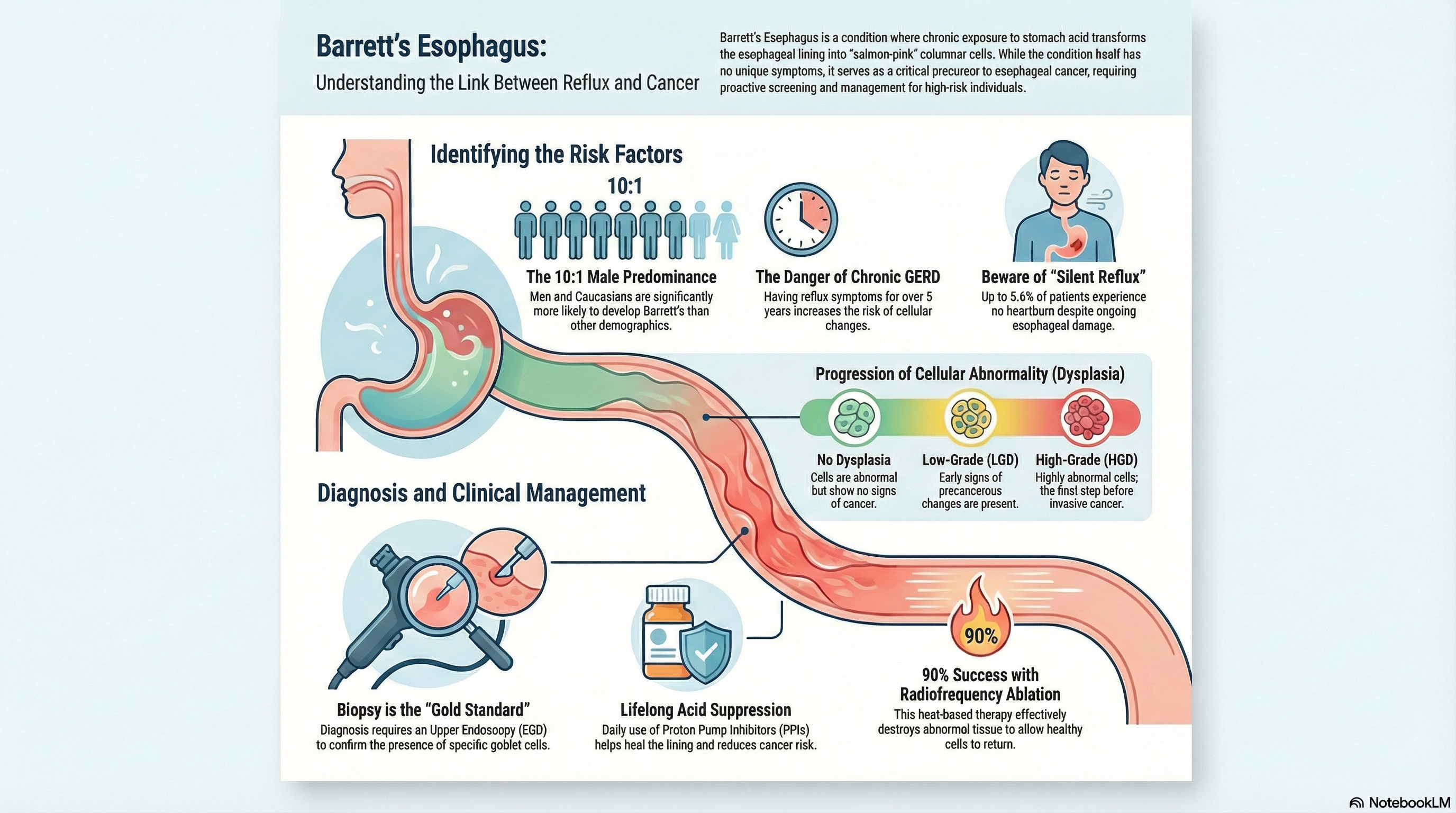
Doctors categorize the condition based on the level of abnormal cell changes (dysplasia) found in biopsies:
-
No Dysplasia: The cells are abnormal but do not show signs of becoming cancer.
-
Low-Grade Dysplasia (LGD): Cells show early signs of precancerous changes.
-
High-Grade Dysplasia (HGD): Cells are highly abnormal and are the final step before invasive cancer.
Causes of Barrett's Esophagus
The primary cause of Barrett’s esophagus is long-standing Gastroesophageal Reflux Disease (GERD). When the valve between the stomach and esophagus fails, acid and bile splash upward, causing chronic injury to the esophageal lining.
Major Risk Factors:
-
Chronic GERD: Having reflux symptoms for more than 5–10 years increases the risk. Approximately 10–15% of chronic GERD patients develop Barrett's.
-
Demographics: The condition is strongly male-predominant (10:1 ratio) and is 10–20 times more common in Caucasians than in African Americans or Asians.
-
Age and Weight: It is most frequently diagnosed in individuals over age 50 and those with central (abdominal) obesity.
-
Lifestyle: Smoking and having a hiatal hernia (where the stomach pushes up through the diaphragm) are significant contributors.
Symptoms of Barrett's Esophagus
It is a common misconception that Barrett's esophagus causes pain or unique physical sensations. In reality, Barrett’s esophagus itself has no specific symptoms. If you have Barrett's, any symptoms you feel are likely caused by the underlying GERD, such as:
-
Frequent heartburn
-
Regurgitation of stomach contents
-
A sour or acidic taste in the mouth
-
Difficulty swallowing
-
Chronic cough or hoarseness
Notably, up to 5.6% of people with Barrett's experience "silent reflux," meaning they have no heartburn symptoms at all despite the damage occurring in their esophagus.
Diagnosis of Barrett's Esophagus
Because there are no specific symptoms, the condition can only be diagnosed through an Upper Endoscopy (EGD). During this procedure, a doctor inserts a thin, flexible tube with a camera into the esophagus to look for "salmon-pink" patches of tissue.
Biopsy Confirmation: Visualization alone is not enough. The doctor must take small tissue samples (biopsies) to look for goblet cells under a microscope. This is the "gold standard" for diagnosis. The American College of Gastroenterology recommends screening for high-risk individuals, particularly men over 50 with multiple risk factors like obesity and smoking.
Treatment of Barrett's Esophagus
Treatment aims to prevent further damage, manage reflux symptoms, and eliminate abnormal cells if they become high-risk.
Medical Management:
-
Proton Pump Inhibitors (PPIs): Daily, lifelong use of PPIs (like omeprazole) is the standard of care. PPIs help heal the esophagus and have been shown to reduce the risk of progression to cancer.
-
Lifestyle Changes: Losing weight, avoiding late-night meals, and elevating the head of the bed are essential to reduce the frequency of acid reflux.
Endoscopic Therapies (For Dysplasia): If precancerous changes (dysplasia) are found, doctors can remove or destroy the abnormal lining:
-
Radiofrequency Ablation (RFA): Uses heat energy to destroy the Barrett’s tissue so that normal squamous cells can grow back. This is successful in over 90% of cases.
-
Endoscopic Mucosal Resection (EMR): The doctor physically removes a nodule or a suspicious area of the lining.
Prevention of Barrett's Esophagus
The most effective way to prevent Barrett’s esophagus is to aggressively manage acid reflux before it causes permanent cellular changes.
-
Control GERD Early: Do not ignore frequent heartburn. If you rely on over-the-counter antacids more than twice a week, consult a doctor about stronger acid-suppression therapy.
-
Weight Management: Reducing abdominal fat is one of the most powerful ways to decrease the pressure that forces acid into the esophagus.
-
Smoking Cessation: Quitting smoking removes a major irritant that weakens the lower esophageal sphincter.
-
Surveillance: If you have already been diagnosed, the best way to "prevent" cancer is to stick to your surveillance schedule. For those with no dysplasia, an endoscopy every 3 to 5 years ensures that any changes are caught early when they are highly treatable.





