What is Ascites?
Ascites is often described by patients as a feeling of "sudden weight gain" or "abdominal bloating." Clinically, it is rarely detectable until at least 1.5 to 2 liters of fluid have accumulated. In extreme cases, known as "tense ascites," the abdomen can hold over 10 liters of fluid, leading to significant discomfort and difficulty breathing.
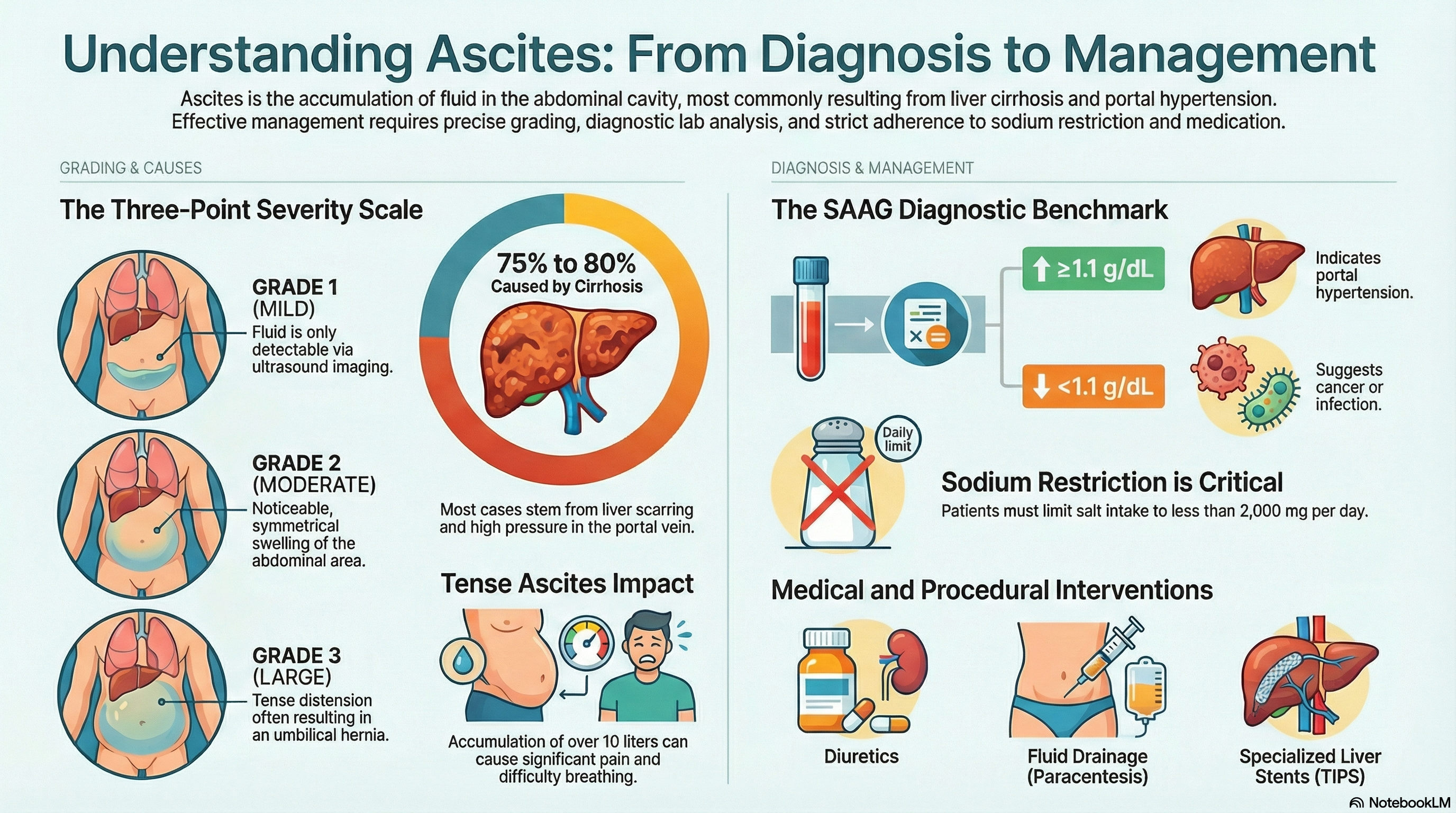
Doctors grade the severity of ascites on a three-point scale:
-
Grade 1 (Mild): The fluid is only visible via an ultrasound.
-
Grade 2 (Moderate): There is noticeable, symmetrical swelling of the abdomen.
-
Grade 3 (Large/Tense): The abdomen is tightly distended, often causing the belly button to push outward (umbilical hernia).
Causes of Ascites
Approximately 75% to 80% of ascites cases are caused by Liver Cirrhosis, often resulting from long-term alcohol use, viral hepatitis (B or C), or Fatty Liver Disease (NASH).
The primary driver is Portal Hypertension, which is high blood pressure in the vein that travels to the liver. This pressure forces fluid out of the blood vessels and into the abdominal space. Other potential causes include:
-
Malignancy (Cancer): Specifically cancers of the ovary, pancreas, stomach, or colon.
-
Heart Failure: When the heart cannot pump efficiently, fluid can back up into the liver and abdomen.
-
Infections: Such as tuberculosis of the abdomen.
-
Kidney Issues: Nephrotic syndrome, where the kidneys leak too much protein into the urine.
Symptoms of Ascites
The symptoms of ascites can develop rapidly or gradually, depending on the cause. Common signs include:
-
Abdominal Distension: A visible increase in waist size and a feeling of fullness or "tightness."
-
Weight Gain: Rapid increase in weight due to fluid retention.
-
Shortness of Breath: Large amounts of fluid push up against the diaphragm, making it hard to take deep breaths.
-
Reduced Mobility: The heavy weight of the fluid can make it difficult to move or walk comfortably.
-
Swelling in the Legs: Often referred to as edema, this frequently accompanies abdominal fluid.
-
Physical Changes: You may notice a "fluid thrill" (a wave-like sensation when the abdomen is tapped) or an umbilical hernia.
Diagnosis of Ascites
Diagnosis begins with a physical exam where a doctor looks for "shifting dullness"—a change in the sound of the abdomen when you roll from your back to your side.
Core Diagnostic Tests:
-
Abdominal Ultrasound: The first-line imaging tool used to confirm the presence of fluid and check the health of the liver and spleen.
-
Diagnostic Paracentesis: A small needle is used to take a sample of the fluid for analysis. This is mandatory for all new cases to check for infection or cancer.
-
SAAG (Serum-Ascites Albumin Gradient): This is the most important lab calculation. A SAAG score of 1.1 g/dL or higher almost certainly points to portal hypertension (liver or heart-related). A score lower than 1.1 g/dL suggests causes like cancer or infection.
-
Fluid Protein Levels: This helps distinguish between cirrhosis and heart failure.
Treatment of Ascites
Treatment focuses on removing the fluid and managing the underlying cause to prevent a recurrence.
Lifestyle and Medications
-
Sodium Restriction: This is the most critical step. Patients are typically restricted to less than 2,000 mg of salt per day to prevent the body from holding onto water.
-
Diuretics: "Water pills" like Spironolactone and Furosemide are used to help the kidneys flush out excess salt and fluid through urine.
Procedures for Severe or Refractory Ascites
-
Large-Volume Paracentesis (LVP): If diuretics are not enough, a doctor may drain several liters of fluid through a needle. If more than 5 liters are removed, patients usually receive an infusion of Albumin (a protein) to prevent a sudden drop in blood pressure.
-
TIPS Procedure: A specialized stent is placed in the liver to lower the blood pressure in the portal vein.
-
Liver Transplant: For those with advanced cirrhosis, a transplant is the only definitive cure.
Prevention of Ascites
Preventing ascites requires managing the health of your liver and cardiovascular system before "decompensation" occurs.
-
Alcohol Cessation: Since alcohol is a leading cause of cirrhosis, avoiding it entirely is the best way to prevent liver damage.
-
Manage Hepatitis: Vaccination for Hepatitis B and seeking treatment for Hepatitis C can prevent the scarring that leads to ascites.
-
Weight and Diet: Managing your weight and blood sugar can prevent non-alcoholic fatty liver disease.
-
Early Detection: If you have known liver disease, sticking to a low-sodium diet and taking prescribed medications can prevent mild ascites from becoming "tense" or infected.
-
Infection Prevention: Patients with low-protein ascites are at high risk for Spontaneous Bacterial Peritonitis (SBP), a life-threatening infection. In these cases, doctors may prescribe preventative antibiotics.





