What is an Anal Fissure?
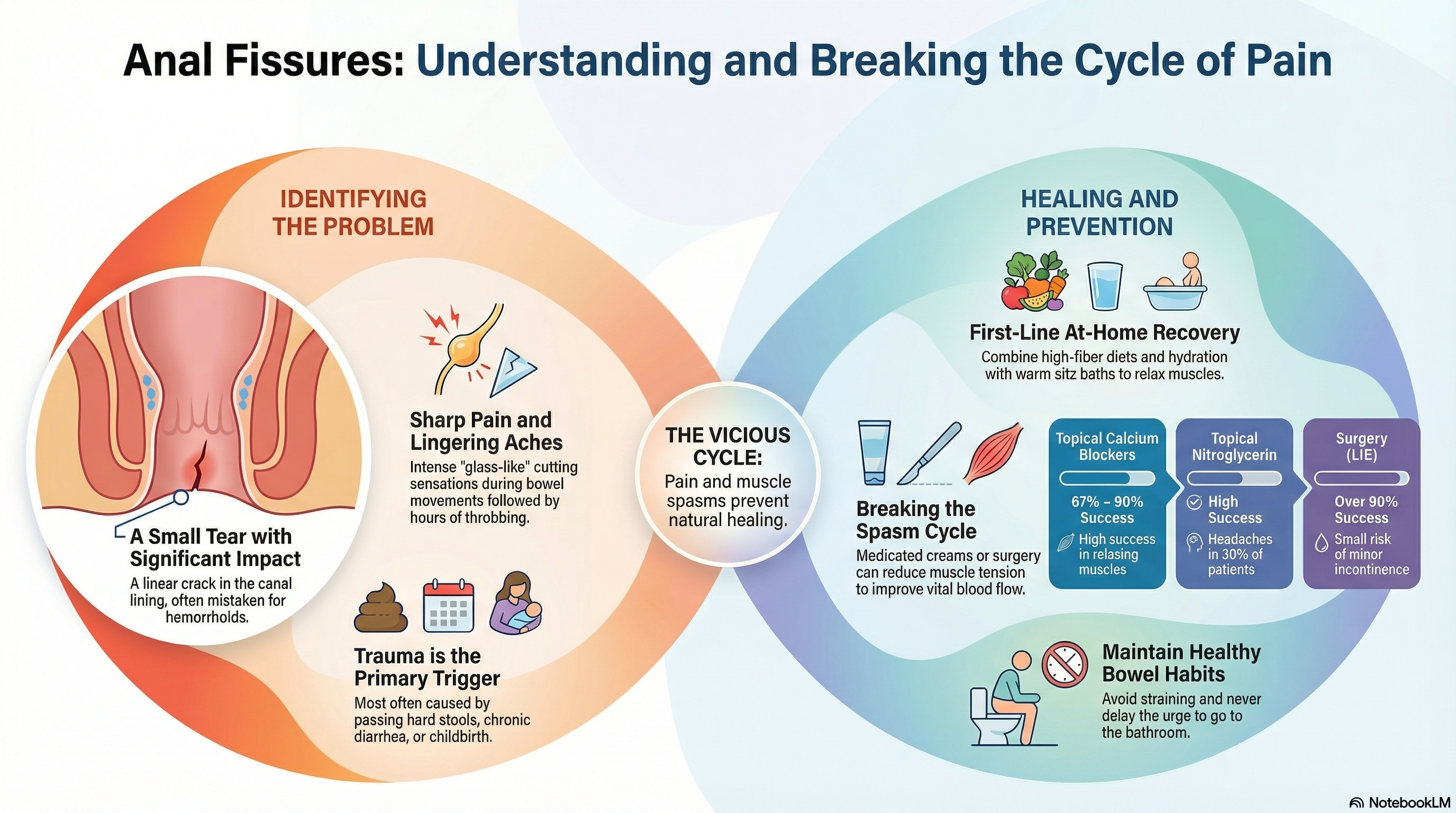
An anal fissure is a small, linear tear or crack in the delicate lining of the anal canal. It is a very common condition that is often mistaken for hemorrhoids, though the two are distinct. Fissures typically occur in the "posterior midline" (the back of the anal opening), an area with relatively low blood flow which makes it more vulnerable to injury and slower to heal.
Doctors generally categorize fissures into two types:
-
Acute Anal Fissures: These are new tears that look similar to a simple paper cut. Most acute fissures heal within six weeks with basic home care.
-
Chronic Anal Fissures: If a tear persists for more than 8 to 12 weeks, it is considered chronic. These often develop deeper cracks, visible muscle fibers, and small lumps of skin known as "sentinel tags" or "anal papillae."
Causes of Anal Fissures
The primary cause of an anal fissure is trauma to the anal canal. When the lining is stretched beyond its capacity, a tear occurs. Common triggers include:
-
Constipation: Passing large, hard, or dry stools is the most frequent cause.
-
Straining: Excessive pushing during bowel movements increases pressure on the anal tissue.
-
Persistent Diarrhea: Frequent, watery stools can irritate and weaken the lining over time.
-
Childbirth: The physical pressure and stretching during vaginal delivery can cause a tear.
-
Anal Sphincter Spasm: An abnormally tight or "spastic" internal anal sphincter muscle can increase tension in the canal and reduce blood flow, making the tissue more prone to tearing.
In some cases, fissures located on the sides (lateral) rather than the midline can be a sign of underlying conditions such as Crohn's disease, certain infections (HIV, syphilis, or tuberculosis), or anal cancer.
Symptoms of Anal Fissures
The symptoms of an anal fissure are usually quite specific and "hallmark" in nature:
-
Sharp, Tearing Pain: Most patients experience a sharp or "glass-like" cutting sensation during a bowel movement.
-
Lingering Ache: After the initial sharp pain, a deep, throbbing ache may persist for minutes or several hours. This is caused by the anal sphincter muscle going into a painful spasm.
-
Bright Red Blood: You may notice a small amount of bright red blood on the toilet tissue or the surface of the stool.
-
Visible Tear or Lump: A visible crack in the skin or a small, fleshy skin tag near the anal opening.
-
Fear of Bowel Movements: Because the pain is so intense, many people try to avoid going to the bathroom, which unfortunately leads to harder stools and worsens the condition.
Diagnosis of Anal Fissures
A diagnosis is primarily "clinical," meaning a doctor can usually confirm a fissure simply by hearing your symptoms and performing a gentle examination.
-
Visual Inspection: By gently spreading the buttocks, a doctor can usually see the tear.
-
Gentle Examination: Because the area is exquisitely tender, a full digital rectal exam (using a finger) or anoscopy (using a small viewing tube) is often avoided during the initial visit to prevent unnecessary pain.
-
Further Investigation: If the fissure is in an unusual location or does not heal with treatment, your doctor may recommend a sigmoidoscopy or colonoscopy to rule out other issues like inflammatory bowel disease.
Treatment of Anal Fissures
The goal of treatment is to break the "vicious cycle" of pain, muscle spasm, and reduced blood flow. By relaxing the muscle and softening the stool, the tissue can finally heal.
At-Home Care (First-Line)
-
Fiber and Fluids: Fiber supplements (like psyllium) and increased water intake are essential to keep stools soft and easy to pass.
-
Sitz Baths: Soaking the area in plain, warm water for 10–15 minutes several times a day helps relax the sphincter muscle and soothe the pain.
Prescription Medications
-
Topical Calcium Channel Blockers: Creams containing nifedipine or diltiazem are often preferred. They have a high success rate (67–90%) in relaxing the muscle to improve blood flow.
-
Topical Nitroglycerin: This ointment helps relax the sphincter but is known to cause headaches in about 30% of patients.
-
Botox Injections: If creams fail, Botox can be injected into the sphincter to temporarily "paralyze" the muscle for a few months, allowing the fissure to heal.
Surgical Options For chronic fissures that do not respond to medication, a procedure called Lateral Internal Sphincterotomy (LIS) is the gold standard. A surgeon makes a small, precise cut in the internal muscle to permanently reduce tension. It has a success rate of over 90%, though it carries a small risk of minor, long-term gas or liquid incontinence.
Prevention of Anal Fissures
Preventing an anal fissure largely involves maintaining healthy bowel habits to avoid trauma to the anal canal.
-
Fiber-Rich Diet: Ensure your diet includes plenty of fruits, vegetables, and whole grains.
-
Hydration: Drink enough water to keep stools soft.
-
Don't Delay: Go to the bathroom as soon as you feel the urge; waiting can cause stools to become hard and difficult to pass.
-
Avoid Straining: Practice "relaxed" bowel movements and avoid sitting on the toilet for prolonged periods.
-
Manage Diarrhea: Treat frequent loose stools promptly, as they can be just as irritating to the anal lining as constipation.





