What is Actinic Keratosis?
Actinic keratosis (AK)—also known as solar keratosis—is a common, rough, scaly patch on the skin caused by years of exposure to ultraviolet (UV) radiation from the sun or tanning beds. These spots are considered precancerous. While many AKs will not become invasive, they are a sign that the skin has sustained significant DNA damage, increasing the risk that some lesions could progress into a type of skin cancer called squamous cell carcinoma (SCC).
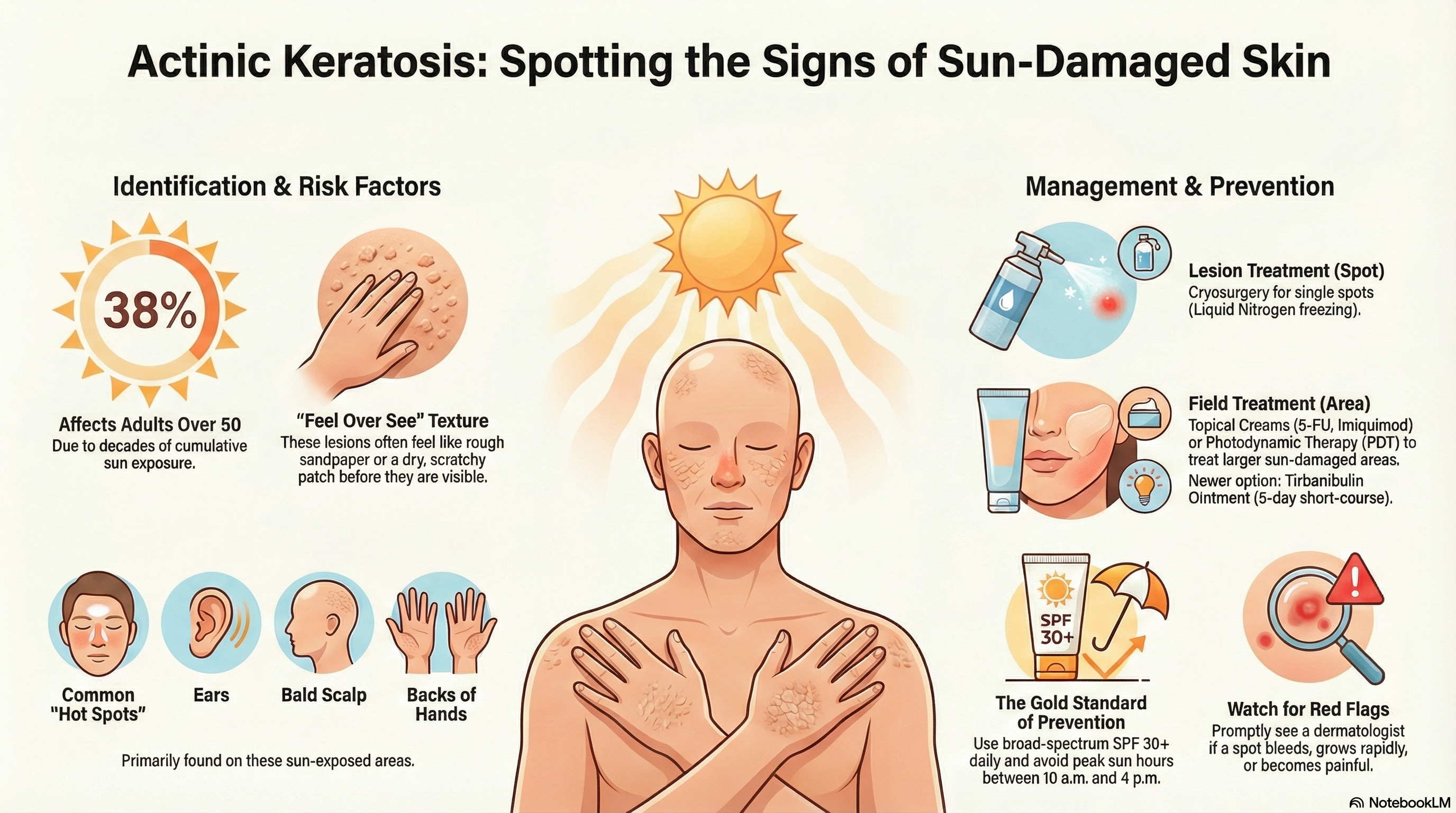
In the United States, AK is very common, affecting nearly 38% of adults over the age of 50. Because it is impossible to predict which specific spot will turn into cancer, dermatologists generally recommend treating all visible lesions.
Causes of Actinic Keratosis
The primary cause of actinic keratosis is cumulative UV radiation exposure. Over time, UV rays damage the DNA of keratinocytes, which are the main cells in the outer layer of your skin. This damage causes the cells to grow abnormally, resulting in the characteristic rough texture.
You are at higher risk if you have:
-
Fair skin: A history of freckling, light-colored eyes, or red/blond hair.
-
Significant sun exposure: A history of outdoor work, outdoor hobbies, or living in high-UV environments.
-
Tanning bed use: Artificial UV light is a major driver of DNA damage.
-
Older age: AKs typically appear after decades of sun exposure.
-
Weakened immune system: Patients who have had organ transplants or are on immune-suppressing medications have a much higher risk.
Symptoms of Actinic Keratosis
Actinic keratoses are often easier to feel than they are to see. They frequently feel like a patch of sandpaper on the skin.
What to look and feel for:
-
Texture: A rough, dry, or scaly patch that may feel scratchy.
-
Appearance: Flat or slightly raised bumps that can be red, pink, brown, or skin-colored.
-
Sensation: Some spots may itch, burn, sting, or feel tender when touched.
-
Location: Most common on "hot spots" like the face, lips, ears, bald scalp, neck, and the backs of the hands or forearms.
Red Flags to Watch For: If a spot becomes painful, starts to bleed, grows rapidly, or becomes significantly thicker, you should see a dermatologist promptly. these changes can indicate that the lesion has already begun transforming into skin cancer.
Diagnosis of Actinic Keratosis
A healthcare provider can usually diagnose actinic keratosis during a physical exam.
Common diagnostic methods:
-
Visual and Physical Exam: The doctor will look at the skin and feel the texture of any suspicious spots.
-
Dermoscopy: Using a handheld magnifying tool to see the structures of the skin more clearly.
-
Skin Biopsy: If a lesion is very thick, painful, or doesn't respond to treatment, the doctor may remove a small sample of the skin to rule out invasive skin cancer.
Treatment of Actinic Keratosis
Treatment is divided into two main categories: treating individual visible spots and treating the entire "field" of sun-damaged skin.
Lesion-Directed Therapy (Spot Treatment)
-
Cryosurgery (Liquid Nitrogen): The most common treatment for isolated spots. The doctor "freezes" the AK, causing it to blister and fall off as new skin grows underneath.
Field-Directed Therapy (Treating the Area) If you have multiple AKs, your doctor may recommend treating the whole area to clear "subclinical" lesions (spots that are damaged but not yet visible).
-
Topical Creams: Prescription medications like 5-fluorouracil (5-FU) or Imiquimod are applied at home for several days or weeks. These cause the damaged areas to become red and crusty before healing.
-
Tirbanibulin Ointment: A newer, shorter-course treatment applied for just 5 days.
-
Photodynamic Therapy (PDT): A light-sensitizing liquid is applied to the skin, followed by exposure to a special blue or red light that kills the abnormal cells.
-
Diclofenac Gel: A gentler topical option used over a longer period (usually 60–90 days).
Prevention of Actinic Keratosis
Prevention is essential to stop new lesions from forming and to reduce your overall risk of skin cancer.
Effective prevention strategies:
-
Sun Protection: Use broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher every day.
-
Protective Clothing: Wear wide-brimmed hats, sunglasses, and long sleeves when outdoors.
-
Seek Shade: Avoid the sun during peak hours, typically between 10 a.m. and 4 p.m.
-
Avoid Tanning Beds: There is no such thing as a "safe" tan from a tanning bed.
-
Supplements: Some studies suggest that taking Nicotinamide (Vitamin B3) 500 mg twice daily may help reduce the number of new AKs in high-risk patients. Always consult your doctor before starting a new supplement.





